
IIEF-subdomain scores either when fixed or randommodels
were applied (Supplementary Fig. 2, panels A and B).
4.
Discussion
The results of this study confirm that TTh improves multiple
aspects of sexual function in hypogonadal patients
[8], as
measured by the frequently used, validated instrument, the
IIEF. The effect of TTh on ED is independent of age and
baseline IIEF score; however, the effect of TTh on ED is
greater in patients with low T levels at baseline and lower in
the presence of metabolic derangements, such as diabetes
and obesity. Since metabolic conditions are often associated
with relatively milder degrees of T deficiency, we cannot
rule out the possibility that the lower apparent efficacy of
TTh in these conditions is due to higher T baseline levels.
According to Rosen et al
[21], the observed mean 2.3-point
(when random model was considered) increase in IIEF-EFD
score should be considered clinically meaningful only in
patients with mild ED and not in those with more severe
forms. Hence, the present data suggests that TTh alone may
be a reasonable treatment option in men with milder ED
[21].
In sexual medicine, it is common to use self-reported
measures to evaluate the subjective perception of a specific
treatment
[21]. Considering that several patient-reported
outcomes (PROs) have been validated and employed in
different studies, the comparison of outcomes is not always
an easy task
[21]. To address questions for which multiple
data sources are in conflict, or fail to reach a consensus, a
meta-analysis is often used. In addition, a meta-analysis is
particularly useful when there are a variety of reports with
low statistical power; pooling data from multiple studies
can improve power and provide a convincing result.
However, results from previous meta-analyses on this
topic have been conflicting
[8,11–13,38] .The different
methods used to compare PROs can explain, at least
partially, the conflicting results.
The most common method to compare results from
different tools on the same outcome is based on treatment-
effect size, calculated according to the method of Hedges
and Olkin
[9]. Interestingly, by applying this method we
recently documented a positive effect of TTh on sexual
function in hypogonadal patients (total T
<
12 nmol/l), in
line with some previous meta-analyses
[11,13]. The present
and previous
[11,13]positive results are in apparent
contrast to those reported by Tserstvadze et al
[38] ,who
did not document any significant effect of TTh on erection,
either alone or when added to PDE5i. It should be
recognized that Tserstvadze et al
[38]used the DerSimonian
and Laird
[39]method for the calculation of the effect size,
whichmay underestimate the true between-study variance,
potentially producing overly narrow confidence intervals
for the mean effect
[40], especially when the between-study
variance is large
[41]. In addition, Tserstvadze et al
[38]analyzed only nine RCTs enrolling mixed eugonadal/
hypogonadal patients, which may have resulted in a
possible inclusion bias. In fact, the present meta-regression
analysis of RCTs grouped on the basis of total T levels as
inclusion criterion indicates that the effect of TTh on IIEF-
EFD score is greater in severe TD, as previously reported
[8] .Qualitative reviews represent an alternative to summa-
rize and discuss available evidence on a specific treatment
endpoint. A recent review considered 48 studies assessing
sexual function or libido as a primary or secondary endpoint
of TTh
[16]. The authors concluded that TTh did not show
consistent benefit for sexual function. However, that review
failed to distinguish between results in eugonadal and
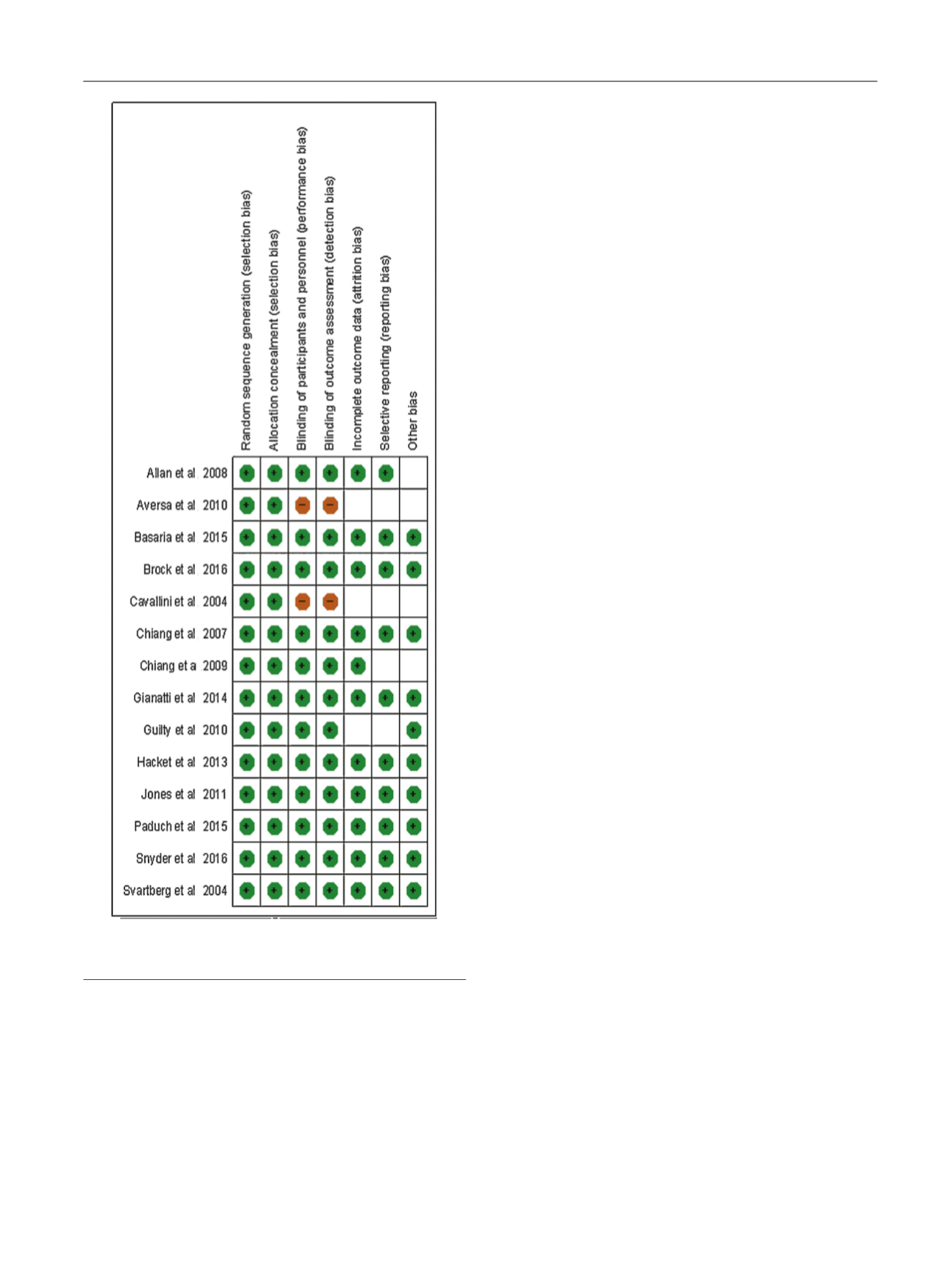
[(Fig._3)TD$FIG]
Fig. 3 – Methodological quality summary: review authors’ judgements
about each methodology quality item for each included study.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 1 0 0 0 – 1 0 1 1
1005
















