
Harmonisation. All patients provided written informed consent to
participate according to the principles of the Declaration of Helsinki.
2.5.
Statistical analyses
Descriptive statistics for categorical variables are reported as frequencies
and percentages. OS was estimated using the Kaplan-Meier product-
limit methods
[10] ;median OS and 95% CI were reported using
Brookmeyer and Crowley methods
[11]; 95% CIs were constructed via
log-log transformation. Hazard ratios for nivolumab versus everolimus
were estimated using the Cox proportional hazards model with
treatment group as a single covariate
[12] .Unstratified hazard ratios
and corresponding 95% CIs were used to generate a forest plot of OS
comprising each subgroup. A forest plot of the unweighted differences in
ORR between nivolumab and everolimus and corresponding 95% CI using
the Newcombe approach was produced across subgroups
[13]. To assess
whether the relationship between OS and treatment differed by various
patient characteristics of interest, we separately tested the interaction
between treatment and each baseline characteristic using a Cox
proportional hazards model. Similarly, for ORR and treatment-related
adverse event (TRAE) rates, the interaction between treatment and each
baseline characteristic was tested using a logistic regression model.
Continuous variables were only used for the interaction test for age (in
years) and duration of prior therapy (in months); for all other subgroups,
categorical variables were used. The analyses were conducted using SAS
version 9 software (SAS Institute Inc., Cary, NC, USA).
3.
Results
3.1.
Patients
The analyses included 410 and 411 patients randomized to
nivolumab and everolimus, respectively, between October
2012 and March 2014 (Supplementary Fig. 1). The
distribution of patients in each subgroup was balanced
between nivolumab and everolimus
( Table 1). The mini-
mum follow-up was 14 mo. The median follow-up among
the 227 nivolumab-randomized and 196 everolimus-ran-
domized patients who had not died at data cutoff was
22 mo (interquartile range [IQR] 20–25) and 22 mo (IQR
20–25). At data cutoff (June 2015), 67 of 406 nivolumab-
treated and 28 of 397 everolimus-treated patients contin-
ued to receive treatment. The number who continued to
receive treatment in each subgroup is shown in Supple-
mentary Fig. 1. Consistent with the overall population, the
primary reason for discontinuation in all subgroups was
disease progression.
The baseline disease characteristics of patients by
subgroups were generally similar between nivolumab
and everolimus (Supplementary Table 1).
3.2.
OS by prognostic risk group
In an assessment of OS by favorable, intermediate, and poor
MSKCC risk groups, median OS was longer in both arms in
patients with better MSKCC scores
( Fig. 1A,
Fig. 2A–C).
Among patients with poor risk who received nivolumab,
median OS was almost double compared
[4_TD$DIFF]
with everolimus
(hazard ratio 0.48;
Fig. 1A,
Fig. 2C). Results for OS by IMDC
risk group were consistent with those for MSKCC risk group
(Supplementary Fig. 2A–C;
Fig. 1A). The mortality rate at
12 mo for all subgroups was lower with nivolumab
compared
[4_TD$DIFF]
with everolimus and was particularly striking
in the poor MSKCC risk group
( Fig. 1 A).
3.3.
OS by age group
Median OS in patients aged
<
65 yr was 26.7 mo (95% CI
21.8–NR) with nivolumab and 19.9 mo (95% CI 17.4–NR)
with everolimus. Median OS in patients aged 65 yr was
23.6mo (95% CI 18.2–NR) with nivolumab and 18.5mo (95%
CI 16.4–21.6) with everolimus.
3.4.
OS by number and site of metastases
Median OS in patients with one site of metastasis was NR
with nivolumab and 29.0 mo (95% CI NR) with everolimus
(Supplementary Fig. 3A, Fig. 1A). In patients with at least
two sites of metastases, median OS was 22.2 mo (95% CI
19.1–26.7) with nivolumab and 17.6 mo (95% CI 15.6–19.8)
with everolimus (Supplementary Fig. 3B, Fig. 1A).
Median OS in patients with bone metastases was
18.5 mo (95% CI 10.2–NR) with nivolumab and 13.8 mo
(95% CI 7.0–16.4) with everolimus (Supplementary Fig. 4A,
Fig. 1A). Median OS in patients with liver metastases was
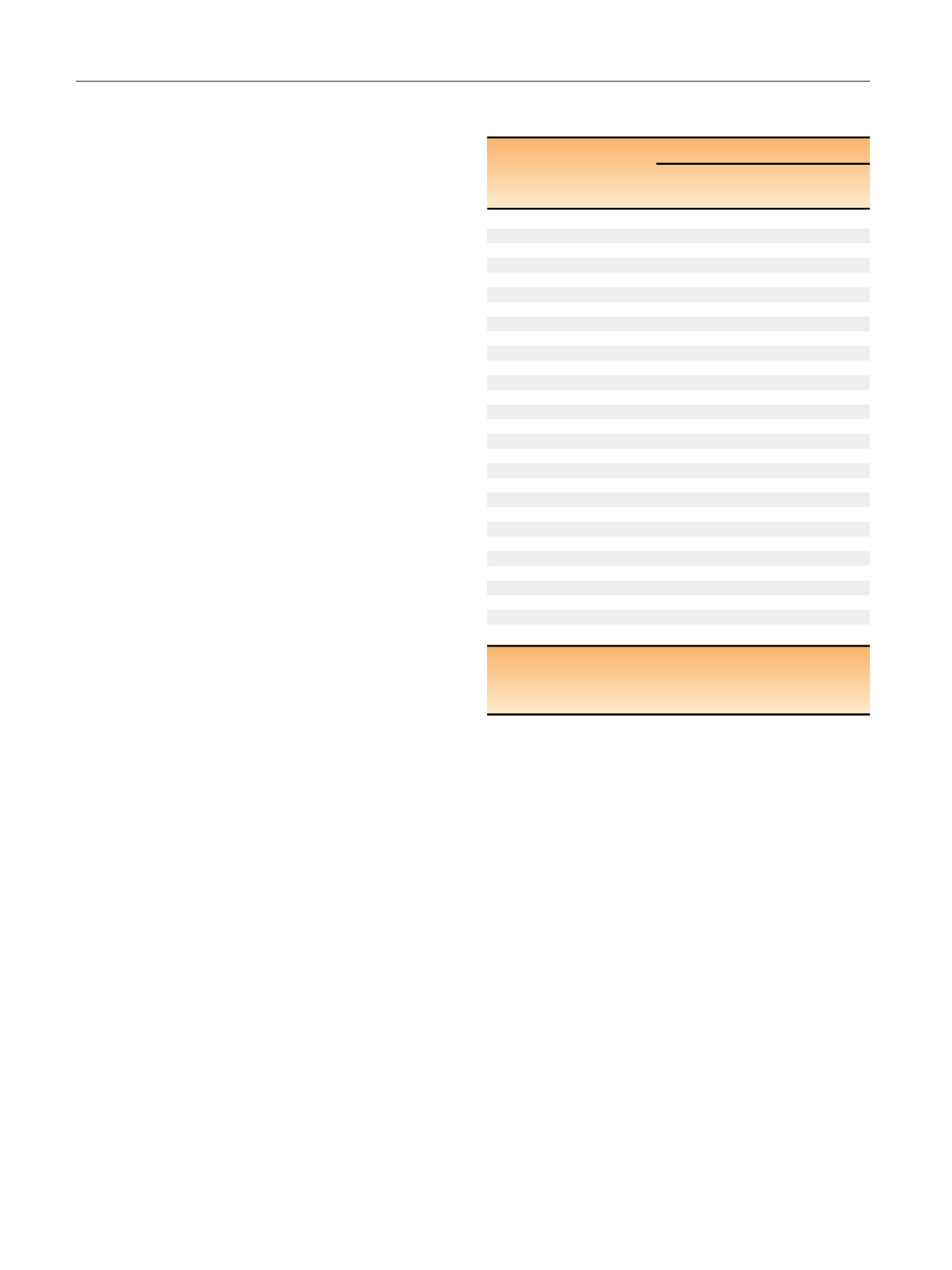
Table 1 – Distribution of randomized patients within each
subgroup
Subgroup
aPatients,
n
(%)
Nivolumab
Everolimus
(
N
= 410)
(
N
= 411)
MSKCC risk score
Favorable
137 (33)
145 (35)
Intermediate
193 (47)
192 (47)
Poor
79 (19)
74 (18)
IMDC risk score
Favorable
55 (13)
70 (17)
Intermediate
242 (59)
241 (59)
Poor
96 (23)
83 (20)
Not reported
17 (4)
17 (4)
Age group
<
65 yr
257 (63)
240 (58)
65 yr
153 (37)
171 (42)
Number of sites of metastases
1
68 (17)
71 (17)
2
341 (83)
338 (82)
Site of metastases
Bone
76 (19)
70 (17)
Liver
100 (24)
87 (21)
Lung
278 (68)
273 (66)
Prior therapy
bSunitinib
257 (63)
261 (64)
Pazopanib
126 (31)
136 (33)
Interleukin-2
42 (10)
37 (9)
Time on first-line therapy
<
6 mo
110 (27)
130 (32)
6 mo
300 (73)
281 (68)
Prior antiangiogenic therapies
1
317 (77)
312 (76)
2
90 (22)
99 (24)
IMDC = International Metastatic Renal Cell Carcinoma Database
Consortium; MSKCC = Memorial Sloan Kettering Cancer Center.
a
Analysis based on case report form data.
b
Patients may have received more than one prior therapy.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 9 6 2 – 9 7 1
964
















