
(
p
= 0.0475). There was no evidence of an interaction for
other subgroups.
3.7.
ORR for each subgroup
ORR favored nivolumab over everolimus in all subgroups,
most notably in patients with poor MSKCC risk, aged at least
65 yr, one site of metastasis, lung metastases, prior
pazopanib therapy, and two prior antiangiogenic therapies
( Fig. 1B). There was no evidence of an interaction between
treatment and each subgroup with ORR.
3.8.
Safety for each subgroup
The incidence of grade 3 or 4 TRAEs was lower in the
nivolumab arm compared
[4_TD$DIFF]
with the everolimus arm across
subgroups
( Table 2). The incidence of grade 3 or 4 TRAEs in
the nivolumab arm was half or less than half the incidence
observed with everolimus in the following subgroups:
favorable MSKCC risk (15% vs 40%); favorable IMDC risk
(20% vs 41%); intermediate IMDC risk (17% vs 36%); at least
65 yr of age (16% vs 39%); one site of metastasis (15% vs
33%); lung metastases (17% vs 37%); prior interleukin-2
therapy (19% vs 38%); at least 6 mo on first-line therapy
(17% vs 37%); and two prior antiangiogenic therapies (17%
vs 36%;
Table 2). There was no evidence of an interaction
between treatment and each subgroup with any TRAE.
4.
Discussion
With a minimum follow-up of 14 mo in previously treated
patients with aRCC, OS and ORR favored nivolumab over
everolimus for multiple subgroups. Within the nivolumab
arm, ORR for most subgroups was similar and consistent
with the overall ORR reported previously
[7].
Median OS was greater and mortality rate was lower
with nivolumab than with everolimus in all MSKCC risk
groups, with the largest difference in patients with poor
risk. The small number of events and short duration of
follow-up in the favorable risk group limited the ability to
observe robust OS differences between arms. The large
difference for poor-risk patients suggests that further
investigation of the characteristics of these patients, such
as tumor biology, is needed to better understand this
finding. One explanation, yet to be formally analyzed, is the
potential presence of a higher mutational load in poor-risk
patients, a phenomenon that in some cases has been
correlated with better efficacy of PD-1 inhibitors. This is
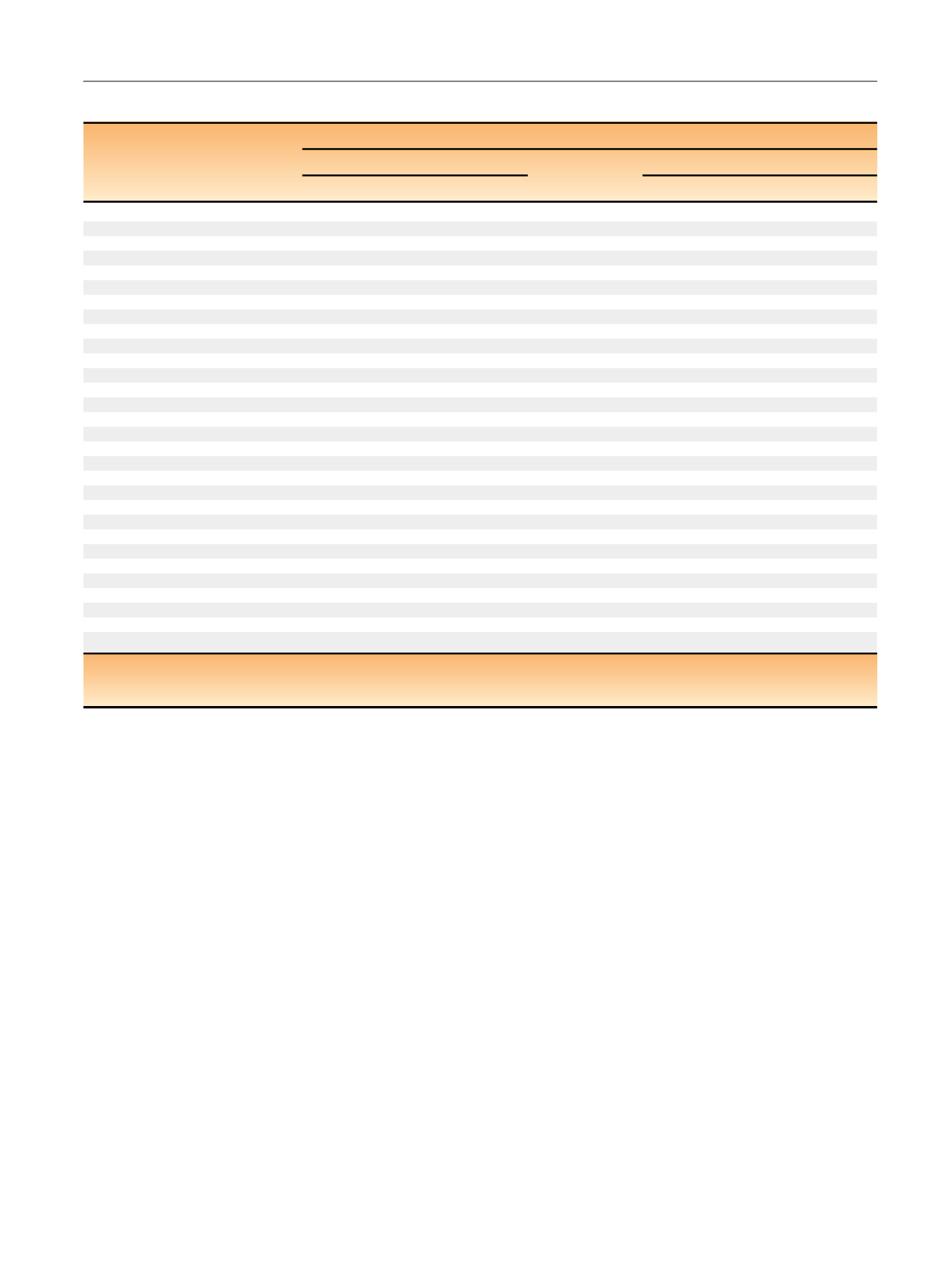
Table 2 – Summary of treatment-related adverse events for patients within each subgroup
Subgroup
Treatment-related adverse events,
n
(%)
Nivolumab
Everolimus
Any grade
Grade 3–4
Any grade
Grade 3–4
All treated patients
319 (79)
76 (19)
349 (88)
145 (37)
MSKCC risk score
Favorable
116 (85)
21 (15)
131 (93)
56 (40)
Intermediate
143 (74)
36 (19)
160 (87)
63 (34)
Poor
60 (78)
19 (25)
58 (80)
26 (36)
aIMDC risk score
Favorable
46 (84)
11 (20)
67 (99)
28 (41)
Intermediate
189 (78)
41 (17)
202 (87)
83 (36)
bPoor
71 (76)
21 (22)
64 (80)
26 (33)
bNot reported
13 (81)
3 (19)
16 (100)
8 (50)
Age group
<
65 yr
200 (79)
51 (20)
199 (86)
81 (35)
a65 yr
119 (78)
25 (16)
150 (90)
64 (39)
Number of sites of metastases
1
57 (85)
10 (15)
62 (90)
23 (33)
2
262 (77)
66 (19)
287 (88)
122 (37)
aSite of metastases
Bone
51 (67)
13 (17)
50 (75)
13 (19)
Liver
78 (80)
22 (22)
72 (85)
31 (36)
bLung
215 (78)
46 (17)
232 (88)
97 (37)
bPrior therapy
Sunitinib
197 (78)
46 (18)
220 (88)
89 (35)
aPazopanib
103 (82)
24 (19)
114 (89)
45 (35)
bInterleukin-2
37 (88)
8 (19)
30 (88)
13 (38)
Time on first-line therapy
<
6 mo
85 (79)
24 (22)
109 (88)
44 (35)
b6 mo
234 (78)
52 (17)
240 (88)
101 (37)
bPrior antiangiogenic therapies
1
240 (76)
61 (19)
264 (87)
111 (37)
b2
76 (85)
15 (17)
85 (90)
34 (36)
bIMDC = International Metastatic Renal Cell Carcinoma Database Consortium; MSKCC = Memorial Sloan Kettering Cancer Center.
a
Two grade 5 events (septic shock and acute bowel ischemia).
b
One grade 5 event.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 9 6 2 – 9 7 1
969
















