
6–8 wk after surgery (all
p
0.02). Moreover, although no
differences were observed in the use of ADT immediately
after surgery between patients in the no RT and postopera-
tive RT groups (21% vs 23%;
p
= 0.3), the use of late ADT at
progression significantly differed between the two groups
(29% vs 53%;
p
<
0.001).
3.2.
Uni- and multivariable analyses predicting CSM
Median follow-up for survivors was 110 mo (interquartile
range: 98–121). Overall, 49 and 77 patients experienced
CSM and OCM, respectively. The resulting 10-yr CSM-free
survival rate was 88%
( Fig. 1 ). At multivariable analyses,
pathologic grade group 4 (hazard ratio [HR]: 2.72; 95%
confidence interval [CI]: 1.43–5.14;
p
= 0.01) and pT3b/4
tumor stage (HR: 2.34; 95% CI: 1.21–4.49;
p =
0.01) were
independently associated with CSM
( Table 2). Pathologic
grade group, pathologic stage, nodal status, surgical
margins, and immediate ADT were included in a model
to predict the 10-yr CSM risk in patients with PSA
persistence after RP. The coefficients to calculate the risk
of CSM are depicted in Supplementary Table 1. A novel
nomogram was then developed to facilitate individual
estimation of the risk of CSM at 10-yr follow-up (Supple-
mentary Fig. 1). At internal validation, the discrimination
accuracy of this model based on pathologic characteristics
and administration of immediate ADT was 67% in our
cohort. Supplementary Figure 2 depicts the calibration
plot.
3.3.
Effect of PSA levels at 6–8 wk after RP on CSM
At univariable Cox regression analyses, the level of
detectable PSA as measured at 6–8 wk after RP was
significantly associated with the risk of CSM (HR: 1.72; 95%
CI: 1.07–2.76;
p
= 0.02) for the overall cohort, such that we
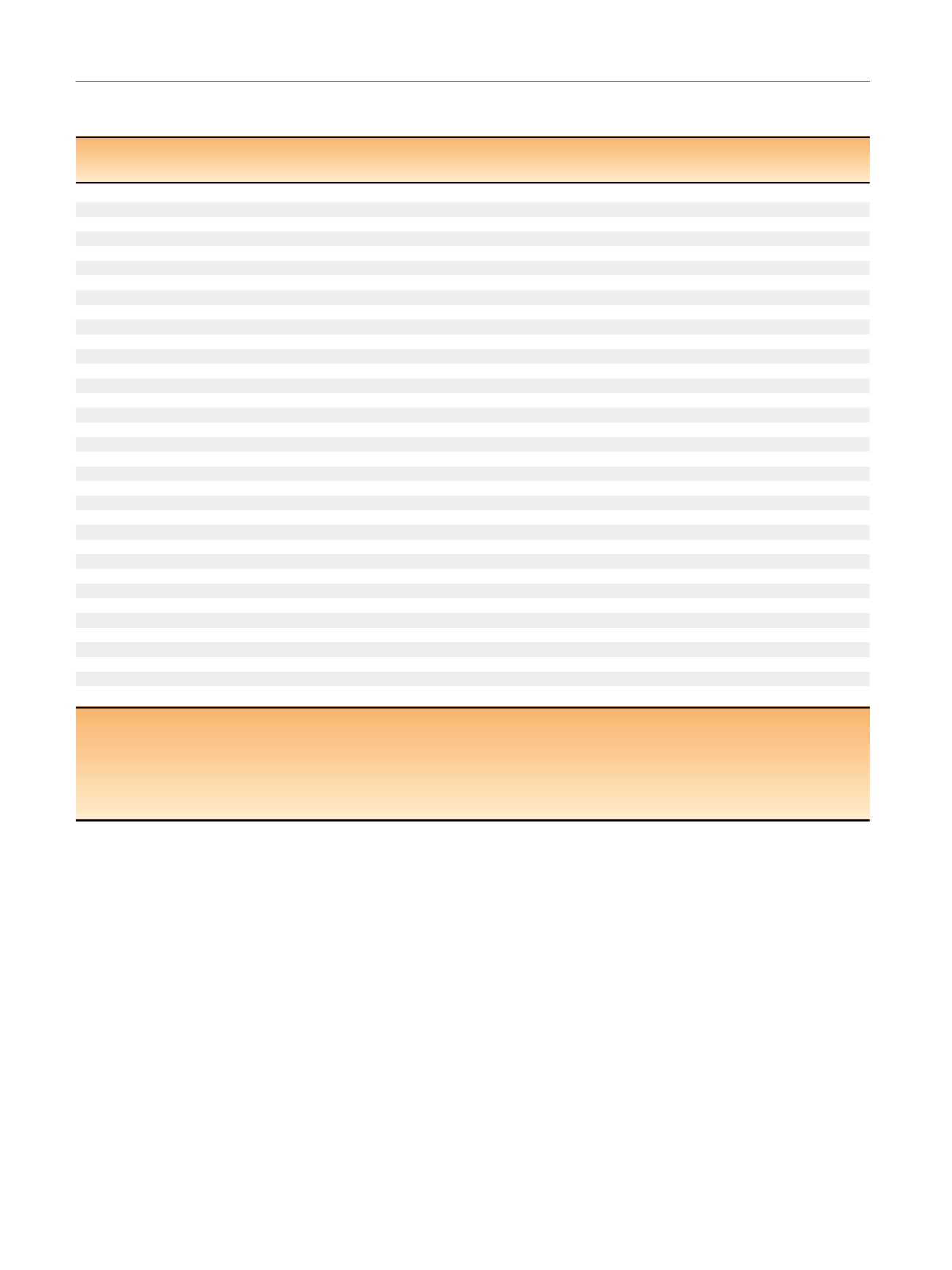
Table 1 – Descriptive statistics of 496 patients with clinically localized prostate cancer treated with radical prostatectomy and extended
pelvic lymph node dissection between 1994 and 2014, who experienced prostate-specific antigen (PSA) persistence
Overall
No RT
Postoperative RT
p
value
(
n
= 496)
(
n
= 245, 49.4%)
(
n
= 251, 50.6%)
Year of surgery
Median (IQR)
2004 (1998–2010)
2000 (1996–2009)
2005 (2000–2010)
<
0.001
Age at surgery (yr)
Median (IQR)
64 (58–68)
65 (59–69)
63 (57–67)
0.002
Preoperative PSA (ng/ml
) aMedian (IQR)
8.5 (5.5–14.3)
7.9 (5.1–13.5)
9.2 (5.9–15.2)
0.02
Preoperative D’Amico risk group (%)
Low
81 (16)
50 (20)
31 (12)
<
0.001
Intermediate
230 (46)
125 (51)
105 (42)
High
185 (37)
70 (29)
115 (46)
Surgical technique (%)
ORP
409 (83)
207 (85)
202 (81)
0.1
RARP
87 (18)
38 (16)
49 (20)
Grade group at final pathology (%)
1
131 (26)
96 (39)
35 (14)
<
0.001
2
115 (23)
50 (20)
65 (26)
3
86 (17)
36 (15)
50 (20)
4
46 (9.3)
21 (8.6)
25 (10)
5
118 (24)
42 (17)
76 (30)
Pathologic stage (%)
T2
231 (47)
138 (56)
93 (37)
<
0.001
T3a
124 (25)
52 (21)
72 (28)
T3b
134 (27)
52 (21)
82 (33)
T4
7 (1.4)
3 (1.2)
4 (1.6)
pN1 (%)
114 (23)
42 (17)
72 (29)
0.01
Positive surgical margins (%)
246 (50)
88 (36)
158 (63)
<
0.001
Number of removed lymph nodes
Median (IQR)
9 (5–15)
9 (5–12)
9 (6–18)
0.06
Number of positive lymph node
s bMedian (IQR)
2 (1–5)
2 (1–5)
3 (1–5)
0.4
First PSA after surgery
Median (IQR)
0.3 (0.2–0.6)
0.2 (0.2–0.5)
0.3 (0.2–0.8)
0.001
ADT concomitant to RT (%)
58 (12)
–
58 (23)
NA
Immediate ADT without RT (%)
51 (10)
51 (21)
–
NA
Late ADT at progression (%)
204 (41)
71 (29)
133 (53)
<
0.001
IQR = interquartile range; ADT = androgen deprivation therapy; ORP = open radical prostatectomy; RARP = robot-assisted radical prostatectomy; NA = not
applicable; RT = radiotherapy.
ADT during RT in the RT group.
Immediate ADT after surgery in the no RT group.
Salvage ADT at progression.
a
Missing in 32 patients.
b
In node-positive patients.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 9 1 0 – 9 1 7
912
















