
3.
Results
RPL accounted for 26 out of 28 of these procedures.
Indications for RPL and RNL included patients who had
failed endourological management (
n
= 13), staghorn cal-
culi (
n
= 5, all partial staghorn), gas containing stone (
n
= 1),
stone in the calyceal diverticulum (
n
= 1), and patients with
renal stone in complex reconstructed urinary tract (
n
= 2).
Reasons for unsuccessful endourological management
included patients that failed ureteroscopy due to calyceal
diverticulum or lower pole positioning. Two patients failed
PCNL, including one who had difficult access due to a
reconstructed urinary tract. Several patients also failed
shockwave lithotripsy due to hard stones as well patients
with abnormal anatomy (eg, cross fused ectopia). Four
patients elected to proceed with a robotic procedure as the
primary approach for their renal stone treatment; two of
these patients were counseled by a fellowship-trained
endourologist.
Table 1provides demographic information on patient’s
undergoing RPL and RNL. Nine patients underwent radiog-
raphy or ultrasound imaging, as these patients were
<
18 yr
of age. Two patients were on anticoagulation, and one
patient was a Jehovah’s Witness. Prior abdominal surgery
was noted in nine patients. The mean maximum stone
diameter was 2.74 cm (standard deviation [SD]: 1.4 cm,
range: 0.8–5.8 cm), with a mean stone volume of 10.6 cm
3
[7_TD$DIFF]
(SD: 19.4 cm
3
, range: 0.18–92.7 cm
3
). The patient with a
0.8 cm stone had multiple lower pole stones, and had
previously failed shock wave lithotripsy.
Table 2summarizes perioperative characteristics and
patient outcomes data. Mean operative time was 182 min
(SD: 61.6, range: 101–300), and mean robotic console time
was 128 min (SD: 56.9, range: 48–245). Use of a retroperi-
toneal approach increased the preconsole operative time.
The longest operation in our series was due to a bilateral
procedure. Mean estimate blood loss was 38 ml (SD: 30.3,
range: 5–100). Complications were recorded in five patients
(18.5%). These included Clavien 1 (
n
= 1), Clavien 2 (
n
= 2),
and Clavien 3b (
n
= 2) complications. No patients under-
went a blood transfusion or developed a postoperative fever
or sepsis.
Postoperative imaging was obtained in 23 patients. Ten
patients had computed tomography (CT), 10 had plain
abdominal radiographs, and three patients underwent an
ultrasound. The complete SFR (ie, zero-fragment rate) after
a single robotic procedure was 26/27 (ie, 96%). In one
patient, a 3-mm RF was noted on postoperative imaging.
Eighteen patients had stents placed intraoperatively, and
12 had intraoperative drains placed. All drains were
removed on postoperative d 1. Stone composition was
varied, including calcium oxalate monohydrate, calcium
oxalate dehydrate, struvite, cysteine, calcium phosphate,
calcium phosphate dihydrate, and carbonate apatatite
stones. Stone composition of the staghorn stones included
one cystine, one calcium oxalate dihydrate, two calcium
oxalate monohydrate, and one calcium phosphate stone. All
were partial staghorn stones.
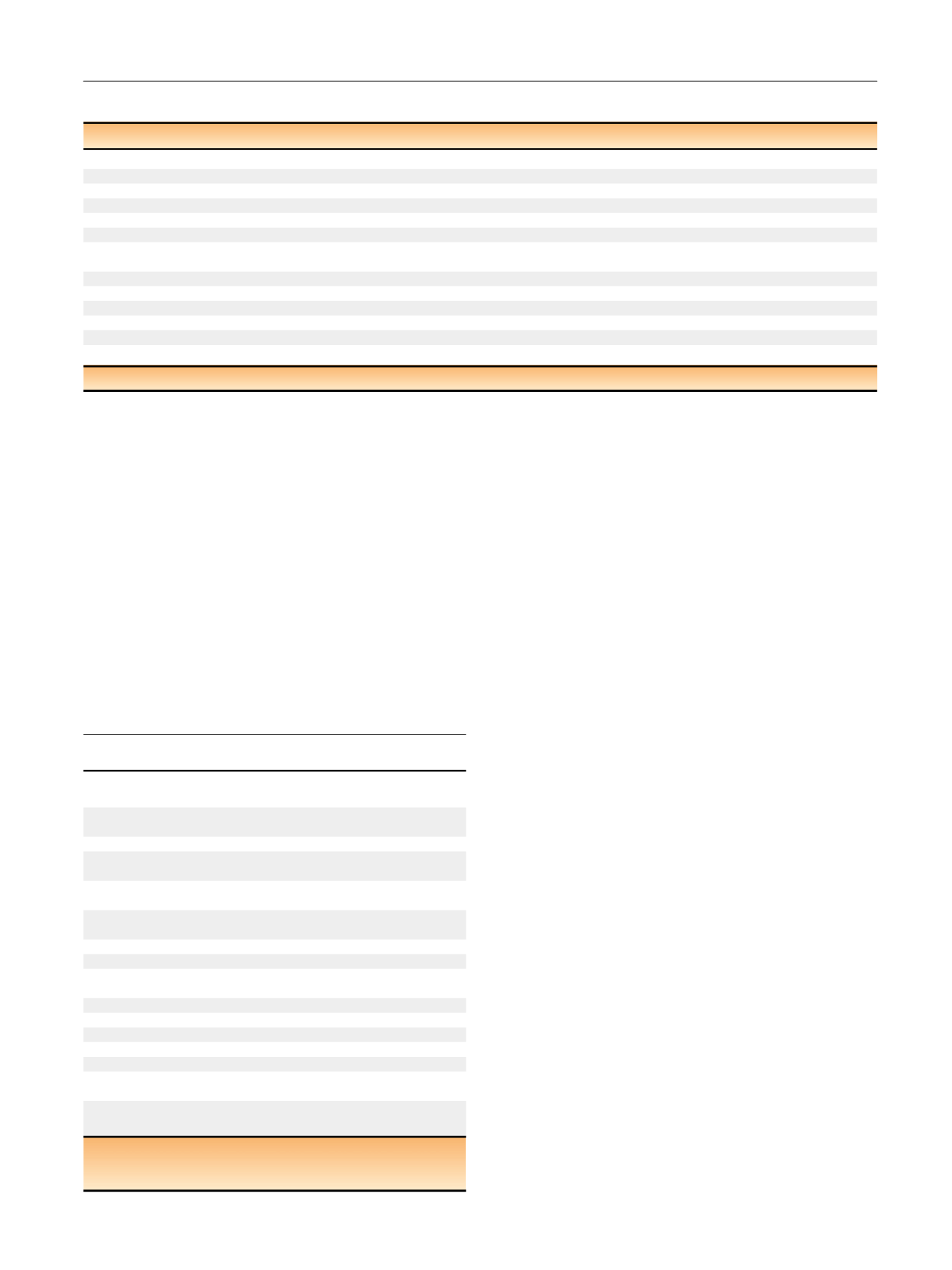
Table 1 – Patient characteristics
No. of patients (no. of procedures)
27 (28)
Mean age,
n
(SD, range; yr)
35.6 (23.2, 1–77)
Laterality
16 right, 10 left, 1 bilateral
Sex
Men: 16, Women: 11
Mean BMI,
n
(SD, range; kg/m
2
)
25.5 (4.6, 17–33.2)
Anticoagulation
2 patients; 1 Jehovah’s Witness
Median ASA score,
n
(SD, range)
2 (0.9, 1–4)
Prior abdominal surgery
Partial gastrectomy (1); lap cholecystectomy (1); gastric bypass (1); umbilical hernia (1);
hysterectomy (1); pyeloplasty (2); robotic pyelolihtotomy (1); augmentation cystoplasty/mitrof/malone (1)
Preoperative imaging
Plain abdominal radiography
7
Plain abdominal radiography and US
2
CT
18
Maximum stone diameter,
n
(SD, range; cm)
2.74 (1.4, 0.8–5.8)
Mean stone volume,
n
(SD, range; cm
3
)
10.6 (19.4, 0.18–92.7)
ASA = American Society of Anesthesiologists; BMI = body mass index; CT = computed tomography; SD = standard deviation; US = ultrasound.
Table 2 – Perioperative characteristics and patient outcomes
Mean operative time, min
(SD, range)
182 (61.6,101–300)
Mean console time, min
(SD, range)
128 (56.9, 48–245)
Mean EBL, ml (SD, range)
38 (30.3, 5–100)
Preop serum creatinine,
mg/dl (SD, range)
0.94 (0.3, 0.5–2.0)
Postop serum creatinine,
mg/dl (SD, range)
0.91 (0.3, 0.4–2.1)
Mean length of stay,
d (SD, range)
1.7 (1.0, 1–4)
Stone-free rate (%)
96
Drain placement (no. of patients)
12
Intraoperative ureteral
stent placement (no. of patients)
17
Follow up, d (SD, range)
275 (369, 12–1320)
Complications
5 (18.5%)
Clavien 1 = 1
Ileus (1)
Clavien 2 = 2
UTI: 2 wk post operatively (1);
Dislodged Malecott catheter (1)
Clavien 3b = 2
Hydronephrosis requiring
[1_TD$DIFF]
PCN + URS
[2_TD$DIFF]
(1)
[3_TD$DIFF]
Encrusted stent (1)
[1_TD$DIFF]
requiring removal
EBL = estimated blood loss; PCN = percutaneous nephrolithotomy;
postop = postoperative; preop = preoperative; SD = standard deviation;
URS = ureteroscopy; UTI = urinary tract infection.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 1 0 1 4 – 1 0 2 1
1017
















