
 [13]
[13]
described a positive trend of increasing MRI suspicion
(analogous to PI-RADS) and detection of high-grade PC, but
not detection of low-risk PC. This demonstrates the
selective nature of prebiopsy mpMRI to detect high-grade
PC. The significantly higher risk of sPC with increasing PI-
RADS scores is also demonstrated in our RMs.
Low PI-RADS or mpMRI suspicion scores harbor a 5–10%
risk of sPC; thus, a biopsy could potentially be avoided
[8,9,13,26] .The remaining risk of missing especially smaller
sPC lesions by mpMRI and MRI-targeted biopsies should be
discussed against a background of maximum security using
additional SB with the inverse risk of low-risk PC over-
detection, as demonstrated by 31% additional non-sPC
found by SB alone in our cohort. If only applying targeted
biopsies, 9% of sPC would have been missed in our dataset.
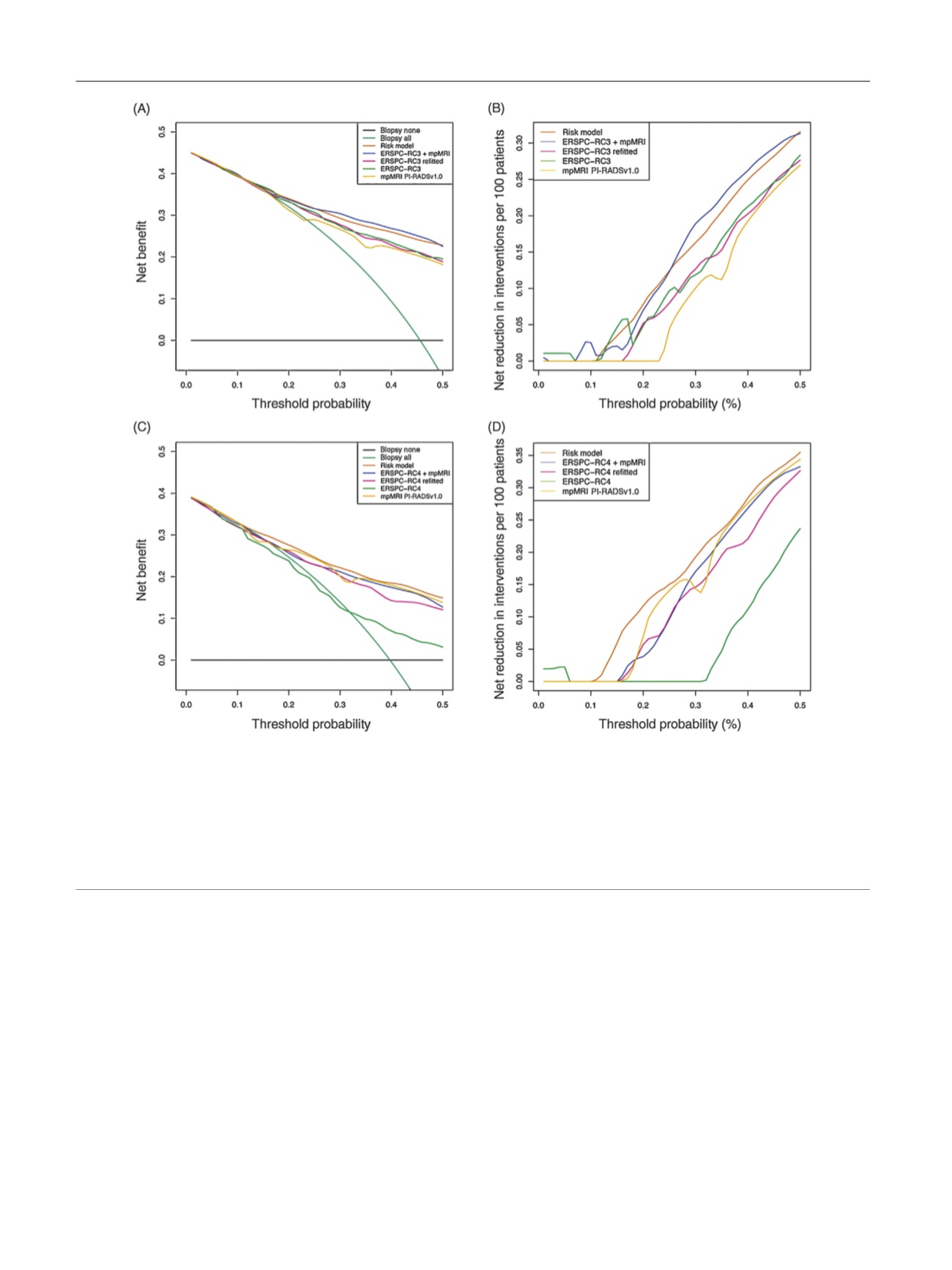
Clinical applicability and usefulness of novel models are
demonstrated by drawing clinical consequences. Using
DCA, we show that both RMs and ERSPC-RC3 combined
with PI-RADSv1.0 improve the clinical decision to biopsy a
patient with a suspicion of sPC, as compared with clinical
parameter models and PI-RADS alone. The RMs and ERSPC-
RC3 + PI-RADSv1.0 provide benefits in the decision to
biopsy a patient for sPC at probability thresholds larger
than 10%. Thus, adding mpMRI to clinical parameter models
is clinically useful for men in whom biopsy is discussed. At
the same time, these integrative approaches enable
avoiding unnecessary biopsies in more patients. From a
practical point of view, at various probability cutoffs, the
combined models demonstrated the best performance of all
prediction tools.
[(Fig._4)TD$FIG]
Fig. 4 – Net decision curve analyses demonstrating the benefit for predicting sPC on biopsy: (A) for biopsy-naı¨ve men and (C) for men after previous
biopsy. The turquoise line is the net benefit of providing all patients with MRI/TRUS fusion biopsy, and the horizontal black line is the net benefit of
providing no patients with biopsy. The net benefit provided by each prediction tool is given (green line for ERSPC-RCs, pink line for refitted ERSPC-
RCs, yellow line for mpMRI Likert PI-RADS, blue line for ERSPC-RC3/4 + mpMRI PI-RADSv1.0, and orange line for the RMs). The net reduction analyses
demonstrate in how many patients a biopsy could be avoided without missing any sPC, based on the decision derived from the RMs (orange lines),
ERSPC-RCs (green lines), refitted ERSPC-RCs (pink lines), mpMRI PI-RADS (yellow lines), and ERSPC-RC3/4 + mpMRI PI-RADSv1.0 (blue lines) in (B) in
biopsy-naı¨ve and (D) postbiopsy men. ERSPC = European Randomised Study of Screening for Prostate Cancer; mpMRI = multiparametric magnetic
resonance imaging; MRI = magnetic resonance imaging; PI-RADS = Prostate Imaging Reporting and Data System; RC = risk calculator; RM = risk model;
sPC = significant prostate cancer; TRUS = transrectal ultrasound.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 8 8 8 – 8 9 6
894
















