
2.5.
Assessment of ERSPC-RCs
The ERSPC-RCs
( www.prostatecancer-riskcalculator.com) are prediction
models based on the data of men in the ERSPC Rotterdam
[16] .ERSPC-RC3
uses TRUS lesions (focal hypoechoic lesions), DRE, TRUS-measured PV,
and PSA. RC4 uses all parameters from RC3 with the addition of a
previously performed biopsy. RC3 calculates the risk of finding any
higher-grade (GS 3 + 4) and/or locally advanced (T stage T2c) PC in a
conventional random biopsy for men who have never been screened and
RC4 for men who have been screened by PSA, but had either no biopsy or
one negative biopsy
[3,16]. In our cohort, all men in the RC4 analyses
underwent previous biopsy. We retrospectively analyzed both RCs on our
entire cohort. ERSPC-RC analyses were calculated manually per single
patient using the original online RCs. These ERSPC-RCs were also used to
combine ERSPC and PI-RADSv1.0 (ERSPC-R3/4 + mpMRI PI-RADSv1.0).
In addition, we constructed clinical RMs by refitting the ERSPC
parameters to our data for biopsy-naı¨ve (RC3 refitted) and previously
biopsied patients (RC4 refitted). Although this parameter is not part of
the published ERSPC RCs, for completeness all our RMs included age,
which is a significant sPC predictor if we analyze the combined RM
cohort of 1015 men (
p
= 0.004). Suspicious TRUS was highly collinear
with DRE and, including it, led to inflation of corresponding standard
errors and instability of effect estimates. Thus, since suspicious TRUS
provided negligible additional information, we excluded it in the models.
Assessment of linearity assumptions of included effect estimates
showed that a log transformation of PSA provides an improved fit. This
captures that the effect of PSA levels is off for large PSA values.
2.6.
Statistical analysis
Patient demographics, MRI, and biopsy results were analyzed descrip-
tively, according to Standards of Reporting for MRI-targeted Biopsy
Studies recommendations
( Table 1)
[17].
First, we performed a multivariate logistic regression analysis to
predict the presence of sPC on biopsy. Similar to the ERSPC-RCs, we
calculated odd ratios for biopsy-naı¨ve and previously biopsied men
( Table 2 ). Regression-based coefficients were used for RM development
( Fig. 1and Supplementary material).
Discrimination of ERSPC-RC3/4, refitted RCs, PI-RADS, ERSPC-RC3/
4 + PI-RADSv1.0, and the novel RMs for sPC was compared using
receiver-operating-characteristic (ROC) area under the curve (AUC)
analysis with internal validation by bootstrapping with 1000 iterations.
Statistical differences between predictive models were analyzed using
the likelihood ratio (LR) test.
The extent of over- or underestimation of predicted probabilities
relative to observed probabilities of sPC was explored graphically using
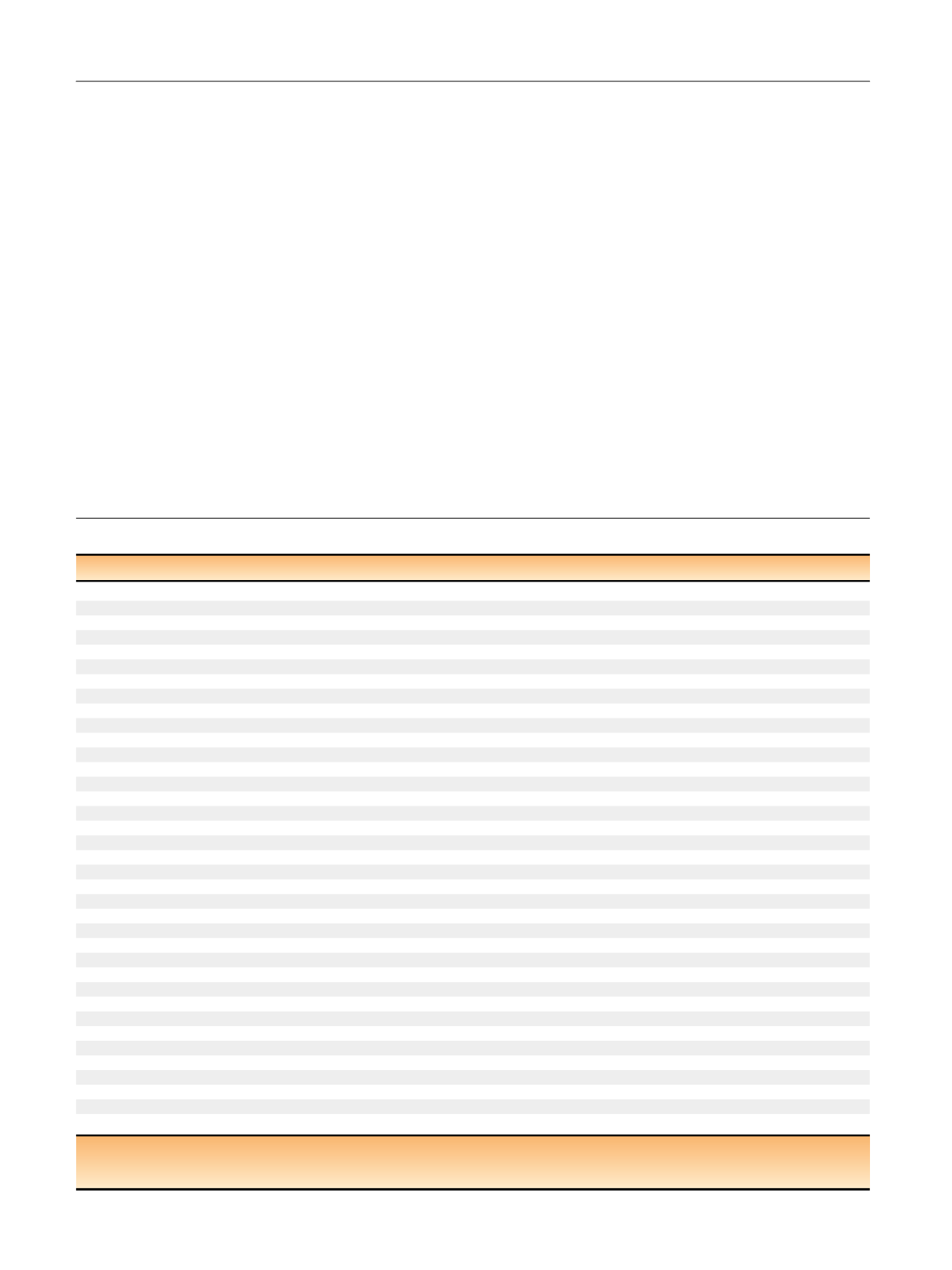
Table 1 – Patient demographics including baseline clinical parameters, MRI, and MRI/TRUS fusion biopsy results according to START criteria
Study population and results according to START criteria
Men included in analysis,
n
1159
Median age, yr (IQR)
65 (60–71)
Median prebiopsy PSA level (IQR), ng/ml
7.3 (5.4–10.6)
Suspicious DRE findings ( T2),
n
(%)
267 (23)
Median prostate volume (IQR), ml
45 (33–64)
Median PSA density (IQR)
0.16 (0.10–0.30)
Men without previous biopsy sessions,
n
(%)
670 (58)
Men with previous biopsy sessions,
n
(%)
489 (42)
Median number of cores in prior biopsy (IQR)
12 (10–14)
Overall previous negative TRUS-guided biopsy sessions in 489 patients,
n
522
Median number of cores in prior biopsy (IQR)
12 (10–14)
Median days from mpMRI to biopsy (IQR)
1 (1–2)
Men with PI-RADS 2 lesions on mpMRI,
n
(%)
863 (75)
Number of lesions PI-RADS 2
1096
Patients with one PI-RADS 2 lesion
733
Patients with
>
1 PI-RADS 2 lesions
130
Number of lesions 2 in primary biopsy
574
Number of lesions 2 in repeat biopsy
522
Overall PI-RADS score 2 lesions,
n
(% of PI-RADS 2)
162 (15)
Overall PI-RADS score 3 lesions,
n
(% of PI-RADS 2)
367 (33)
Overall PI-RADS score 4 lesions,
n
(% of PI-RADS 2)
346 (32)
Overall PI-RADS score 5 lesions,
n
(% of PI-RADS 2)
221 (20)
Biopsies per patient, median (IQR)
27 (24–29)
Systematic biopsies per patient, median (IQR)
24 (22–25)
FTB per patient and per lesion, median (IQR)
3 (2–5), 2 (1–3)
Overall detection rate of prostate cancer,
n
(%)
732 (63)
Detection rate of prostate cancer in primary biopsy,
n
(%)
417 (62)
Detection rate of prostate cancer in repeat-biopsy,
n
(%)
315 (64)
Men with significant prostate cancer,
n
(% of all men)
489 (42)
Nonsignificant prostate cancers in systematic 24-core transperineal biopsy alone,
n
(% of all nonsignificant prostate cancers)
72 (31)
Nonsignificant prostate cancers in FTB alone,
n
(% of all nonsignificant prostate cancers)
20 (10)
Significant prostate cancers in systematic 24-core transperineal biopsy alone,
n
(% of all significant prostate cancers)
47 (9)
Significant prostate cancers in FTB alone,
n
(% of all significant prostate cancers)
62 (13)
Proportion of cores positive for clinical significant prostate cancer in systematic biopsies
2445/24 728
Proportion of cores positive for clinical significant prostate cancer in FTB
1052/3562
Mean number of cores taken for one diagnosis of significant prostate cancer from systematic biopsies
11
Mean number of cores taken for one diagnosis of significant prostate cancer from targeted biopsies
3
n
= number; IQR = interquartile range; PSA = prostate-specific antigen; DRE = digital rectal examination; TRUS = transrectal ultrasound;
mpMRI = multiparametric magnetic resonance imaging; MRI = magnetic resonance imaging; PI-RADS = Prostate Imaging Reporting and Data System;
FTB = fusion targeted biopsy; START = Standards of Reporting for MRI-targeted Biopsy Studies.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 8 8 8 – 8 9 6
890
















