
Neither cases of retrograde ejaculation were recorded, nor
impairment of erectile function as determined using the IIEF
questionnaire was documented. Similar results confirming
technical success and suggesting efficacy without
compromising sexual function were obtained in additional
uncontrolled pilot studies
[68,74–82] .Two prospective
RCTs were conducted for direct comparison of PAE with the
reference method TURP
[83,84]. Both studies observed
significant treatment outcomes for both procedures as
compared to baseline values, but TURP was always superior
considering urodynamic parameters such as Q
max
and
postvoid residual urine volume. Improvement of LUTS as
determined by IPSS and QoL was more pronounced after
TURP and reduction of prostate volume was significantly
more efficient after TURP than PAE. Another 1-yr matched-
pair analysis compared PAE to open prostatectomy for
management of LUTS due to BPE and reported significantly
superior functional outcomes as determined by IPSS, QoL,
Q
max
, and postvoid residual urine volume for open
prostatectomy
[85]. Altogether, available data indicate a
high technical success rate and suggest some clinical benefit
for the treatment LUTS.
However, a recently published systematic review with
meta-analysis and meta-regression on available data
concluded that PAE should still be considered an experi-
mental approach
[86]. RCTs of good quality are still missing
to justify this interesting technique on an elective indication
and are currently ongoing. The selection of LUTS patients
who will benefit from PAE still need to be defined. It is
important to stress, that all of the presented novel
minimally invasive treatment modalities above are able
to specifically target the critical areas of bladder outlet
obstruction secondary to BPE. In contrast, PAE impacts the
entire prostate without the option for focused and
controlled action on bladder outlet obstruction. This may
explain the higher clinical failure rate compared to
reference methods like TURP and commonly observed
complications like acute urinary retention in almost 26% of
cases
[84]. Management of LUTS due to BPE must be
handled by urologists. A multidisciplinary team approach of
urologists and radiologists is mandatory as the basis for
future RCTs of good quality in order to integrate this
promising option in the spectrum of efficient minimally
invasive treatment options.
[29_TD$DIFF]
4.
Conclusions
Many novel and innovative techniques have arrived with
the main objective to establish effective strategies for the
relief of male LUTS with a more favourable safety profile.
Intraprostatic injectables have fallen short of expectations
in clinical trials. PRX302 is the only substance that showed
safety and efficacy in a phase 3 trial. Mechanical devices
like the PUL procedure are supported by evidence of good
quality and it was clearly demonstrated that it provides
rapid and long-term relief of LUTS without compromising
sexual function. TIND has recently been introduced with
promising functional outcomes, but further RCTs are
warranted to fully evaluate its potential in the field of
minimally invasive therapies. New ablative approaches
like the image guided robotic waterjet ablation
(AquaBeam) or procedures based on convective water
vapour energy (Rezu- m) are currently under evaluation.
Further trials are needed to demonstrate their therapeutic
potential and advantages compared to standard techni-
ques. With regard to PAE, a substantial high clinical
failure rate and a specific spectrum of complications not
common after urologic interventions are of concern. A
multidisciplinary approach with both urologists and
radiologist is necessary to define its role as a potential
option among the established treatment modalities.
A synopsis of the main characteristics of the emerging
treatment modalities is depicted in
Table 1. Fundamental
research in the development of novel techniques and
their clinical assessment have progressed substantially,
and will show which approach will pass the test of
time.
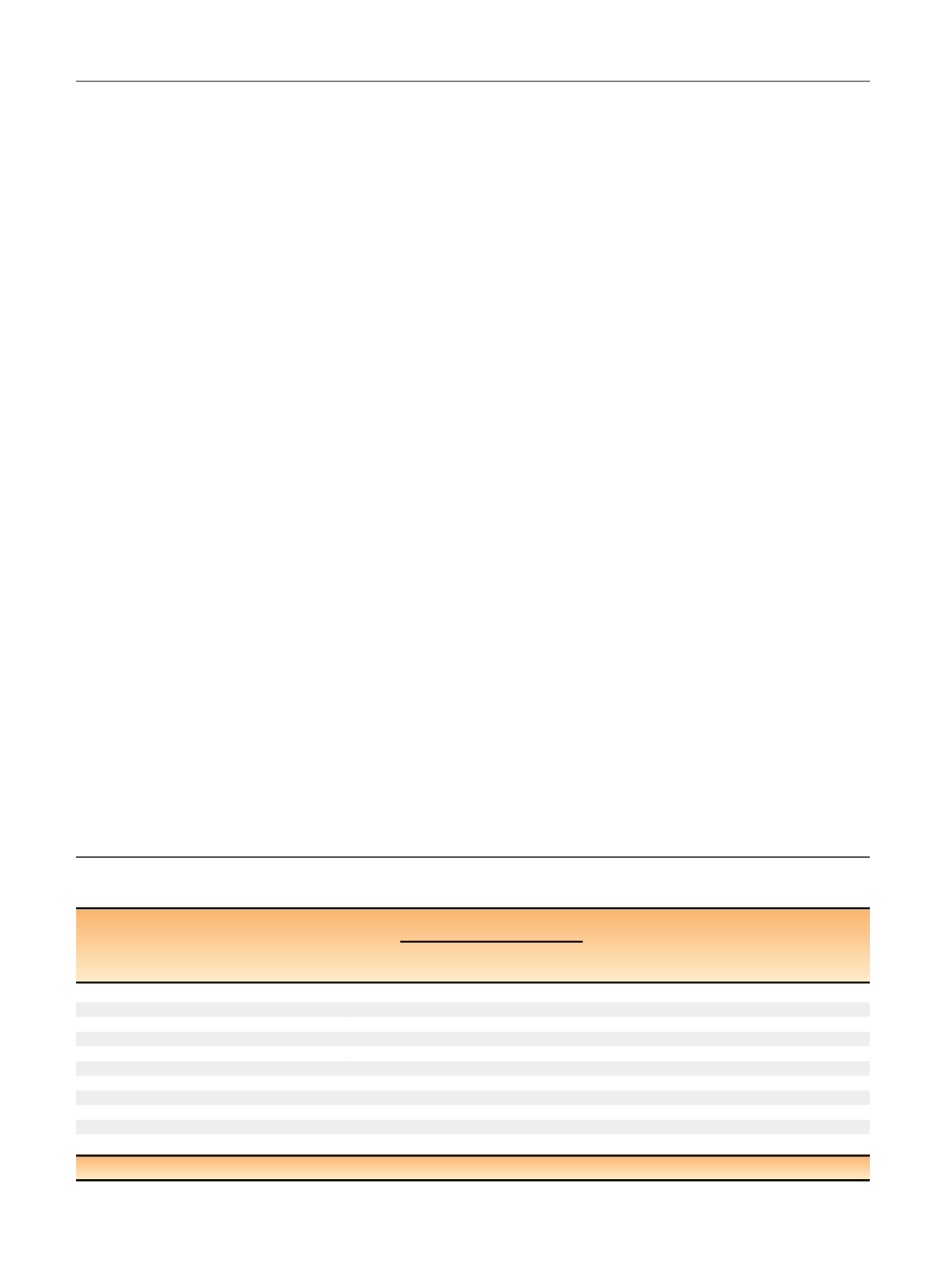
Table 1 – Synopsis of main characteristics of emerging minimally invasive treatment options for male lower urinary tract symtoms
(contraindications refer to specific prostatic configurations; sexual function includes both erectile and ejaculatory function)
Minimally
invasive treatment
Feasability Safety Efficacy
Durability
Preservation of
sexual function
Approval
(Relative)
contraindication
Short-term
(1 yr)
Mid-term
(3 yr)
Long-term
(5 yr)
Intraprostatic injection
BoNT/A
+
+
–
NX1207
+
+
–
PRX302
+
+
+
+
NA
NA
+
No
No
Mechanical devices
TIND
+
+
+
+
NA
NA
NA
No
Middle lobe
Urolift
+
+
+
+
+
+
+
FDA, NICE PV
>
100 cc
[1_TD$DIFF]
, middle lobe
Ablative techniques
AquaBeam
+
+
+
NA
NA
NA
+
No
PV
>
100 cc
[1_TD$DIFF]
, middle lobe
Rezu˜m
+
+
+
+
NA
NA
+
No
No
Prostatic artery embolization +
+
+
+
NA
NA
NA
No
No
BoNT/A = botulinum neurotoxin A; NA = no data available; PV = prostate volume; TIND = temporary implantable nitinol device; + = confirmed; – = failed.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 9 8 6 – 9 9 7
994
















