
and safety of AquaBeam were confirmed
[58]. One-year
results of a prospective single-armmulticentre phase 2 trial
on 21 men supported safety and efficacy of aquablation
[59]. Duration of the procedure averaged 38 min and mean
aquablation treatment time was 5 min. In 20 patients,
catheters were removed within the 1st 24 h of the
procedure and most patients were discharged 1 d after
the procedure. No cases of urinary incontinence, erectile
dysfunction, or retrograde ejaculation were reported. After
12 mo, IPSS was reduced from 23.0 points at baseline to
6.8 points (
p
<
0.001). An increase from 8.7 ml/s to 18.3 ml/
s in Q
max
was demonstrated (
p
<
0.0001). At 12 mo the
average prostate size showed a reduction from57 cc to 35 cc
(
p
<
0.001). This first clinical experience provided encour-
aging results, but further modifications of the AquaBeam
systemwill be necessary. Anatomical prostatic features like
a prostate volume
>
100 cc and the presence of a large
middle lobe are currently limitations to the technology and
therefore considered relative contraindications. Further
RCTs are underway to evaluate efficacy, durability, and
safety of this innovative approach.
[23_TD$DIFF]
3.9.
Convective water vapour energy (WAVE) ablation: The
Rezu- m system
[24_TD$DIFF]
3.9.1.
Basic principle
Ablation using the Rezu- m system (NxThera, Inc., Maple-
Grove, MN, USA) takes advantage of the thermodynamic
principle of convective energy transfer, which is in contrast
to conductive heat transfer techniques as applied by known
minimally invasive treatment options like transurethral
microwave therapy or transurethral needle ablation. In this
case, radiofrequency power is used to create thermal energy
in the form of water vapor, which in turn deposits the stored
thermal energy when the steam phase shifts to liquid upon
cell contact. The Rezu- m system is composed of a generator
containing a radiofrequency power supply to create water
vapor from sterile water and a single-use transurethral
delivery device. The tip of the delivery device contains an
18-gauge polyether ether ketone needle where 12 small
emitter holes spaced circumferentially at 120
8
intervals
allow for targeted dispersion of water vapor into the tissue.
The injection is performed at approximately 103
8
and
exceeds slightly interstitial pressure. Due to the convective
properties of water vapor the steam disperses rapidly and
homogenously through the tissue interstices and releases
stored thermal energy onto prostatic tissue effecting cell
necrosis. Of note, when the transition zone is treated,
energy deposition is contained within the zonal anatomy of
the prostate. Histologic and imaging studies using Gadolin-
ium-enhanced magnetic resonance imaging after treatment
provided evidence that coalesced thermal lesions were
limited to the transition zone without extension to the
peripheral zone, bladder, rectum or striated urinary
sphincter
[60,61]. It was shown that 6 mo after treatment
the total prostate volume was reduced by 28.9% and the
resolution of thermal lesions as determined with Gadolini-
um-enhanced magnetic resonance imaging was almost
complete
[61] .The procedure can be performed in an office
based setting with minimal pain management. Under
cystoscopic guidance, the needle is positioned at 90
8
to
the area of interest and a 9-s injection of water vapor is
achieved. Usually, one to three injections are needed for
each lateral lobe and one to two injections may be delivered
[(Fig._3)TD$FIG]
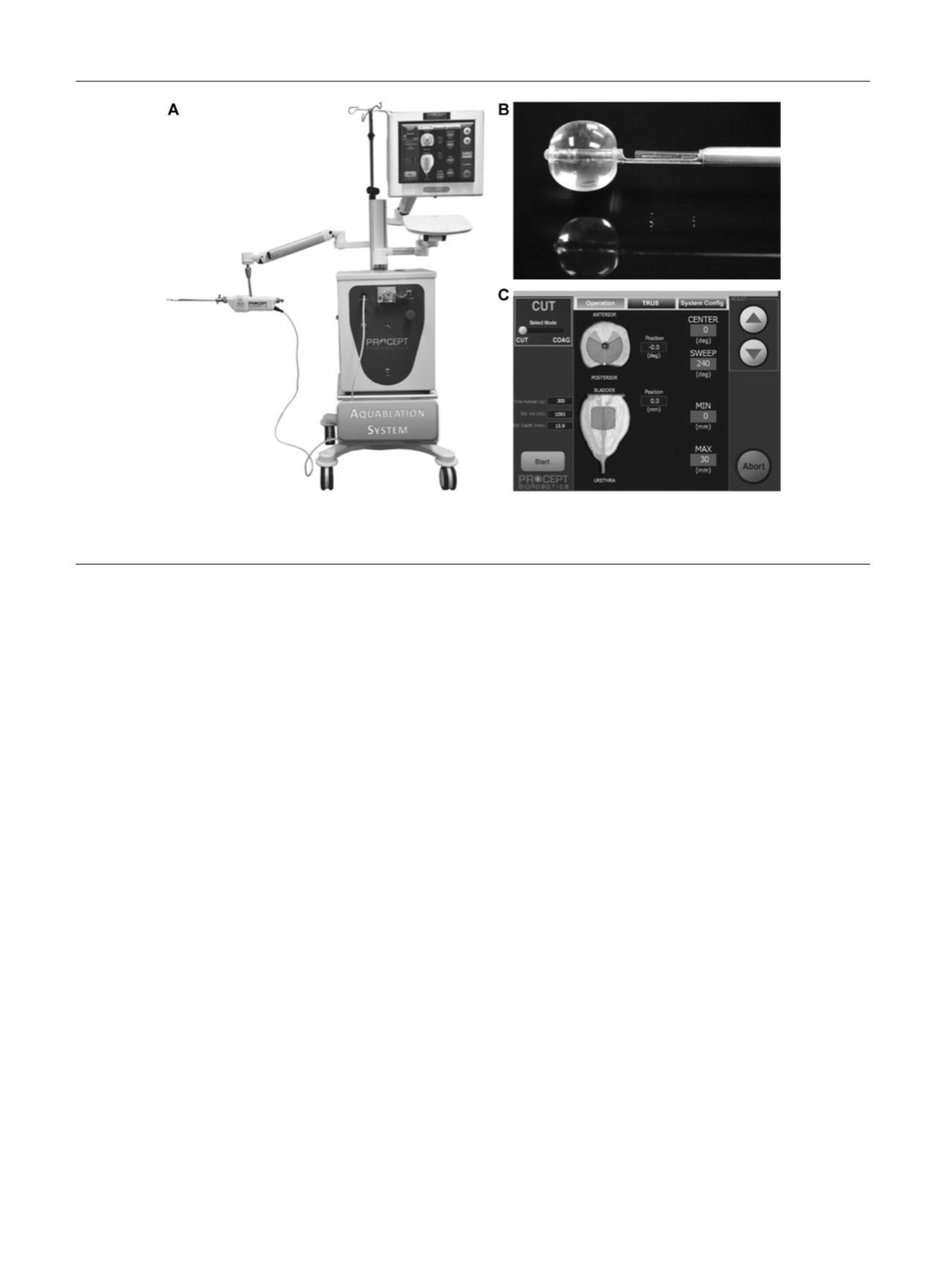
Fig. 3 – Aquablation – image guided robotic waterjet ablation: AquaBeam. (A) The Aquablation system is composed of three main components: the
console, the robotic hand-piece, and a transrectal ultrasound probe. (B) Tip of the Aquablation probe. The terminal balloon is retracted for sealing of
the bladder neck. The trough enables Aquablation. (C) Graphic control interface.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 9 8 6 – 9 9 7
992
















