
K
is obtained ratiometrically and is not directly connected to the
corresponding level of serum PSA, except for the fact that both
K
and the
PSA concentration generally increase with cancer. The
K
parameter can
be used directly to classify patients via binary analysis (eg, cancer
present or absent), or converted by logistic regression to an individual
risk probability
[2_TD$DIFF]
, KR, for the two study indications.
2.3.
IsoPSA clinical performance evaluation
Two key clinical performance objectives were tested: discriminatory
power between PCa (Gleason 6) and benign prostate conditions (cancer
vs no cancer), and between high-grade PCa (Gleason 7) and low-grade
cancer (Gleason 6) or benign histology (high grade). Two receiver
operating characteristic (ROC) analyses were developed to evaluate the
discriminatory power of
K
. Since the subjects were already selected for
biopsy, the sample size was calculated according to the length of the 95%
confidence interval (CI) for the estimated sensitivity using the formula
N
c
¼
Z
2
a
=
2
V
u
ð Þ
L
2
; where
N
c
is one-half of the cancer cohort,
u
is the expected
sensitivity estimate,
L
denotes the desired one-half of the CI, and
V
u
ð Þ ¼
u
1
u
ð Þ
(V. Kipnis, personal communication). Setting the expected
sensitivity estimate to
u
= 0.95 and the 95% CI to 0.9–1.0, making
L
= 0.05, and with
Z
a
/2
=
Z
0.025
= 1.96, we obtain
N
c
70 and thus a total
sample size of 140. More directly, the confidence interval of the area
under the ROC curve (AUC) for each ROC analysis was determined using
1000 bootstrapped samples with replacement. A calibration curve for
each model was constructed to explore the relationship between the
observed and predicted outcome. Decision curve analysis (DCA)
[16]was
used to investigate the clinical utility of the models in comparison to the
two extreme limits of all-biopsy (as for the current patient cohort) and
no-biopsy, as well as against the modified Prostate Cancer Prevention
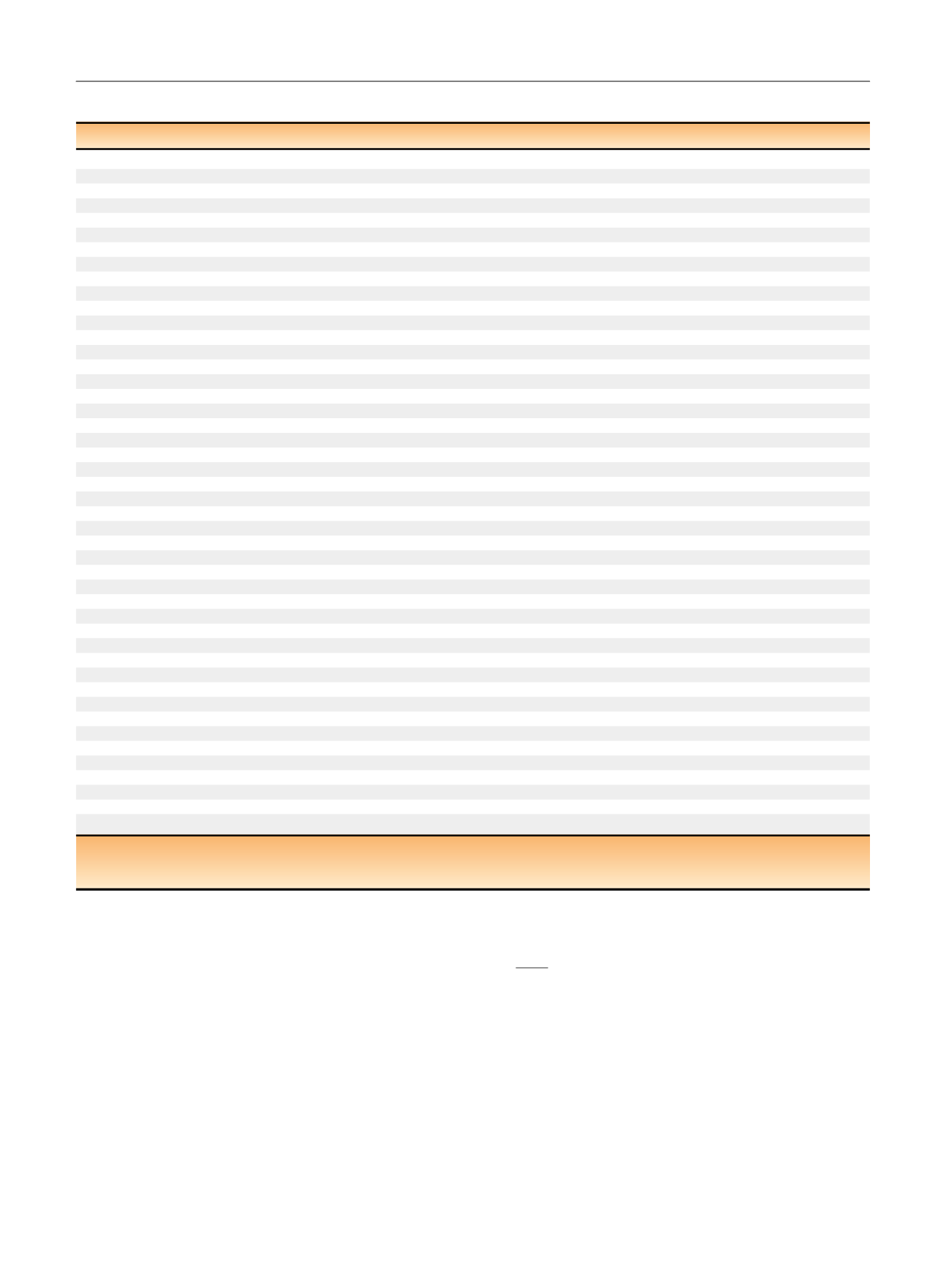
Table 1 – Demographic data and clinical parameters for the patient cohort by clinical status category
Negative biopsy
Low-grade PCa (Gleason 6)
High-grade PCa (Gleason 7)
Number
122
51
88
Age at blood draw (yr)
63.00 (58–69)
63. 00 (57–70)
64.65 (60–72)
<
50 yr
5 (4)
0 (0)
2 (2)
50–75 yr
115 (94)
48 (94)
76 (86)
>
75 yr
2 (2)
3 (6)
10 (11)
Race
African American
12 (10)
6 (12)
12 (14)
Caucasian
108 (89)
44 (86)
72 (82)
Hispanic
0 (0)
0 (0)
0 (0)
Other
0 (0)
0 (0)
3 (3)
Unknown
2 (2)
1 (2)
1 (1)
Abnormal digital rectal examinatio
n a13 (11)
38 (75)
19 (22)
Prior prostate biopsy
35 (29)
17 (33)
19 (22)
Medications
None
79 (64.8)
41 (8.4)
72 (81.8)
Other/unspecified
5 (4.1)
2 (3.9)
1 (1.1)
5-
a
reductase
2 (1.6)
0 (0.0)
1 (1.1)
a
-Blockers
32 (26.2)
8 (15.7)
13 (14.8)
5
a
-Reductase +
a
-blockers
4 (3.28)
0 (0.0)
1 (1.1)
Total PSA (ng/ml)
5.68 (4.45–7.89)
5.45 (4.29–7.54)
7.45 (5.83–11.04)
2–4 ng/ml
18 (15)
11 (22)
6 (7)
4–10 ng/ml
87 (71)
36 (71)
52 (59)
10–25 ng/ml
14 (11)
2 (4)
25 (28)
>
25 ng/ml
2 (2)
1 (2)
4 (5)
Free PSA (ng/ml)
1.02 (0.66–1.41)
0.74 (0.56–1.29)
0.79 (0.56–1.29)
Prostate volume (g)
49 (40–60)
40(31–44)
40 (30–50)
Free/total PSA ratio (%)
17 (13–22)
14 (11–18)
10 (8–16)
KR-CNC (%)
36 (28–51)
52 (37–74)
74 (51–87)
Quintile 1 (
<
30.5%)
43 (35)
7 (14)
2 (2)
Quintile 2 (30.5–42.1%)
36 (30)
10 (20)
6 (7)
Quintile 3 (42.1–56.2%)
19 (16)
15 (29)
19 (22)
Quintile 4 (56.2–79.6%)
17 (14)
8 (16)
27 (31)
Quintile 5 (
>
79.6%)
7 (6)
11 (22)
34 (29)
KR-HG (%)
16 (12–27)
34 (17–49)
50 (27–70)
Quintile 1 (
<
10.0%)
43 (35)
7 (14)
2 (2)
Quintile 2 (10.0–16.4%)
36 (30)
10 (20)
6 (7)
Quintile 3 (16.4–28.6%)
19 (16)
15 (29)
19 (22)
Quintile 4 (28.6–53.8%)
17 (14)
8 (16)
27 (31)
Quintile 5 (
>
53.8%)
7 (6)
11 (22)
34 (39)
Biopsy Gleason grade
6
46 (100)
0 (0)
3 + 4
0 (0)
44 (61)
4 + 3
0 (0)
15 (21)
8
0 (0)
8 (11)
9
0 (0)
3 (4)
10
0 (0)
2 (3)
PCa = prostate cancer; KR =
K
risk value result; CNC = cancer versus no cancer; HG = high-grade PCa versus benign/low-grade PCa.
Data are presented as median (interquartile range) for continuous variables and
n
(%) for categorical variables.
a
Recent digital rectal examination result not available for 35 of the patients included.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 9 4 2 – 9 4 9
944
















