
The main limitation of the present study regarding
exposure was the nonrandom allocation to type of ADT,
with ensuing selection bias for younger and healthier men
with less advanced cancer to receive GnRH agonists. Thus,
despite the semi-ecologic design, residual confounding
cannot be excluded. Since the NPCR does not register date of
treatment, we started follow-up 3 mo after the date of
diagnosis, at which time point 90% of men diagnosed in a
later calendar period had received their primary
[16_TD$DIFF]
treatment.
There was no information on duration and adherence to
GnRH agonists, but it is rare for men with advanced prostate
cancer to stop ADT. We also lacked information on smoking,
body mass index, and use of cardiovascular drugs. Limita-
tions regarding the endpoints are that we used administra-
tive data from the Patient Registry and the Cause of Death
Registry to define CVD events. However, several investiga-
tions have shown high validity for diagnosis of CVD (eg,
heart failure, acute myocardial infarction, and stroke)
[34– 37]and there are no reasons to assume a systematic bias
according to type of ADT. Strengths of the study included
the nationwide, population-based cohort of men with
comprehensive data from several high-quality health care
registers
[23–26]as well as the use of three different
statistical methods to assess the association between type
of ADT and risk of CVD.
In accordance with previous studies, men treated with
orchiectomy for prostate cancer in the current study were
older, had more comorbidities, and presented with more
advanced stage of prostate cancer compared to men treated
with GnRH agonists
[12,17–19]. A meta-analysis including
12 randomised clinical trials found no difference in overall
or prostate cancer survival between men treated with GnRH
agonists and orchiectomy
[38]. Accordingly, the higher rate
of prostate cancer death among men treated with orchiec-
tomy in our study was the result of more advanced cancer in
comparison to men on GnRH agonists, which in turn
influenced the risk of CVD. The semi-ecologic study design
decreased the influence of an individual’s cancer character-
istics and general health on selection of ADT, but did not
fully eliminate it. However, the risk of CVD among men
treated in units with high use of GnRH agonists was similar
to that in units with low use.
In separate analyses, we determined the net and crude
probability of death from CVD, prostate cancer, and other
causes. Crude probability is estimated using a competing-
risks analysis in which death from causes other than the
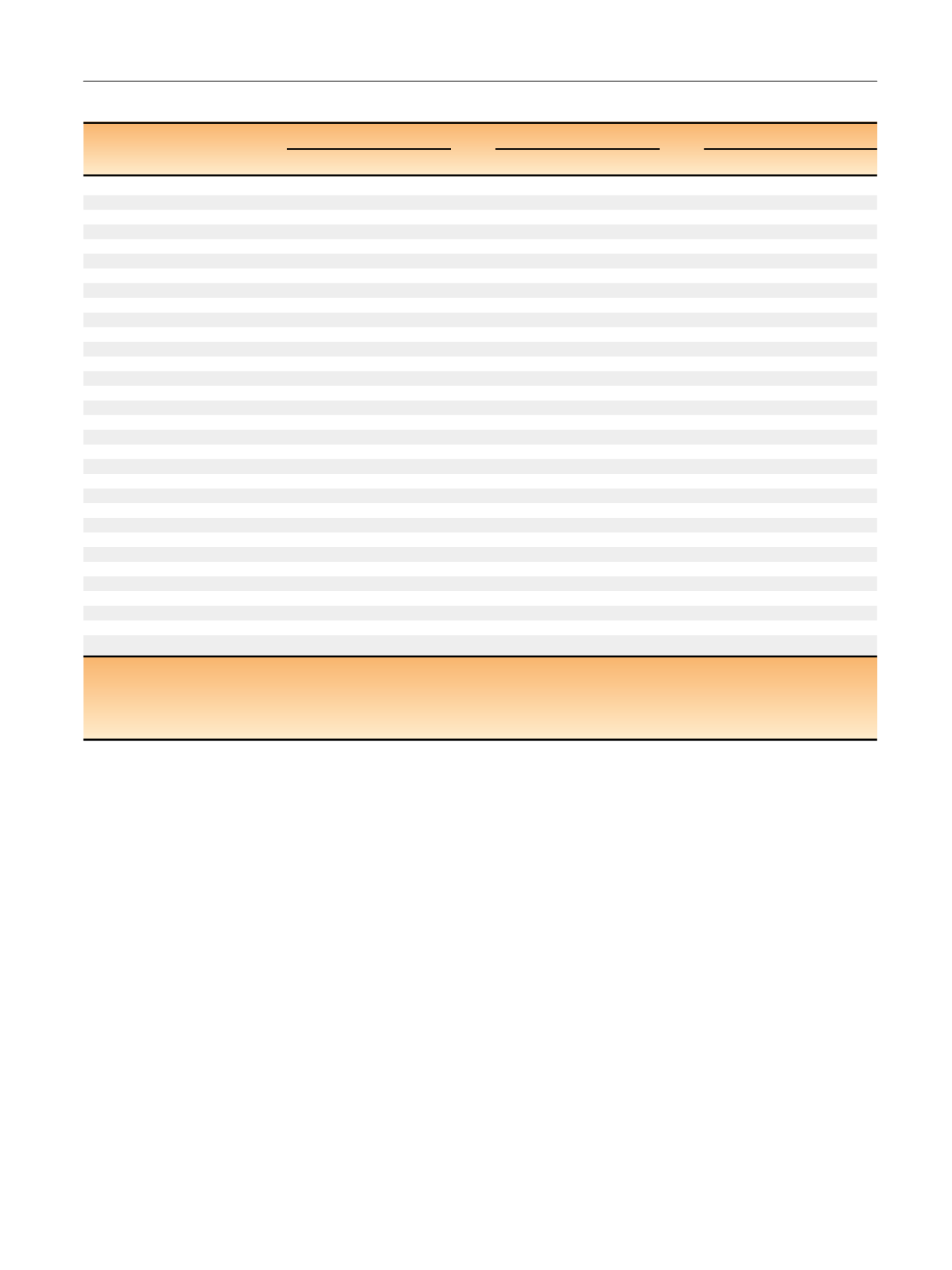
Table 3 – Multivariable Cox proportional hazards model
s *[12_TD$DIFF]
of cardiovascular disease, fractures, and diabetes
CVD
a (n
= 5145)
Fracture (
n
= 1262)
Diabetes
b (n
= 705)
HR (95% CI)
p
value
HR (95% CI)
p
value
HR (95% CI)
p
value
Primary treatment
Orchiectomy
1.00 (reference)
1.00 (reference)
1.00 (reference)
GnRH agonists
1.02 (0.96–1.09)
0.5
0.91 (0.80–1.04)
0.16
1.02 (0.85–1.22)
0.8
Year of diagnosis (continuous)
1.02 (1.00–1.04)
0.017
1.11 (1.07–1.15)
<
0.001
1.02 (0.98–1.07)
0.3
T stage
T1
1.00 (reference)
–
1.00 (reference)
–
1.00 (reference)
–
T2
0.97 (0.86–1.09)
0.6
0.88 (0.70–1.09)
0.2
1.20 (0.86–1.67)
0.3
T3
0.97 (0.87–1.09)
0.6
0.89 (0.72–1.11)
0.3
1.22 (0.89–1.68)
0.2
T4
1.02 (0.89–1.17)
0.8
1.07 (0.82–1.40)
0.6
1.19 (0.80–1.76)
0.4
M stage
M0/MX
1.00 (reference)
–
1.00 (reference)
–
1.00 (reference)
–
M1
1.00 (0.93–1.08)
0.9
1.32 (1.14–1.53)
<
0.001
1.06 (0.87–1.29)
0.6
Prostate-specific antigen
<
25 ng/ml
1.00 (reference)
–
1.00 (reference)
–
1.00 (reference)
–
25–
<
50 ng/ml
0.97 (0.89–1.05)
0.5
1.04 (0.88–1.23)
0.7
0.83 (0.67–1.04)
0.11
50–
<
100 ng/ml
1.03 (0.95–1.12)
0.5
1.00 (0.84–1.19)
1
0.86 (0.68–1.08)
0.19
100–
<
200 ng/ml
1.07 (0.97–1.18)
0.19
1.22 (1.01–1.49)
0.043
0.83 (0.63–1.09)
0.18
200–
<
500 ng/ml
1.09 (0.98–1.22)
0.11
1.11 (0.89–1.38)
0.4
1.25 (0.96–1.63)
0.10
500 ng/ml
1.05 (0.93–1.18)
0.4
1.01 (0.79–1.29)
0.9
0.93 (0.68–1.28)
0.7
Gleason score
2–6
1.00 (reference)
–
1.00 (reference)
–
1.00 (reference)
–
7
1.01 (0.93–1.08)
0.9
1.09 (0.94–1.27)
0.2
1.18 (0.96–1.44)
0.12
8–10
1.10 (1.01–1.18)
0.022
1.09 (0.93–1.27)
0.3
1.20 (0.97–1.49)
0.09
Previous CVD
cNo
1.00 (reference)
–
1.00 (reference)
–
1.00 (reference)
–
Yes
2.03 (1.90–2.17)
<
0.001
1.04 (0.90–1.21)
0.6
1.11 (0.91–1.35)
0.3
Previous hypertension
cNo
1.00 (reference)
–
1.00 (reference)
–
1.00 (reference)
–
Yes
1.13 (1.00–1.28)
0.051
1.14 (0.88–1.49)
0.3
1.33 (0.93–1.91)
0.12
Previous diabetes
cNo
1.00 (reference)
–
1.00 (reference)
–
Yes
1.50 (1.32–1.71)
<
0.001
1.43 (1.08–1.88)
0.012
CVD = cardiovascular disease; GnRH = gonadotropin-releasing hormone.
*
All models performed with age as time-sale.
a
A total of 564 (11%) men had hypertension as their first CVD event.
b
Only men without previous diabetes before their prostate cancer diagnosis.
c
Within 5 yr before prostate cancer diagnosis.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 9 2 0 – 9 2 8
925
















