
but not those with high-risk tumors (
p
[9_TD$DIFF]
interaction =
[10_TD$DIFF]
0.02).
A similar result was observed for walking; among men
with lower-risk tumors, those who walked for 7 h/wk
had a 47% lower risk of PCSM compared with those who
walked for 1–3 h/wk (HR: 0.53, 95% CI: 0.33–0.86,
p
trend = 0.04).
For postdiagnosis recreational PA
( Table 4), there was a
significantly lower risk of PCSM for men engaging in 17.5
MET-h/wk of recreational PA compared with those engag-
ing in 3.5–
<
8.75 MET-h/wk (HR: 0.69, 95% CI: 0.49–0.95,
p
trend = 0.006). Further adjustment for prediagnosis METs
did not change the results (not shown). Postdiagnosis
walking, but not other recreational PA, was inversely
associated with PCSM, although the HRs were not statisti-
cally significant. The inverse association for recreational PA
did not differ by tumor risk category (
p
[9_TD$DIFF]
interaction =
[13_TD$DIFF]
0.1).
We also examined recreational PA in relation to CVD
mortality and all-cause mortality. Engaging in 17.5 MET-
h/wk of recreational PA before diagnosis was associated
with a 20% lower risk of CVD mortality (HR: 0.80, 95% CI:
0.67–0.96,
p
trend = 0.008; Supplementary Table 2). In
postdiagnosis analyses, the inverse trend (
p
trend = 0.01) for
recreational PA was primarily driven by men in the bottom
category who had a significantly higher risk of CVD
mortality (HR: 1.49, 95% CI: 1.11–2.00) rather than by
those in the top category (HR: 0.89, 95% CI: 0.69–1.14). A
similar result was seen for walking but not for other
recreational PA. For all-cause mortality, same comparison of
prediagnosis recreational PA ( 17.5 vs 3.5–
<
8.75 MET-h/
wk) was associated with 12% lower risk (HR: 0.88, 95% CI:
0.80–0.97,
p
trend
<
0.0001; Supplementary Table 3). In
postdiagnosis analyses, engaging in 17.5 MET-h/wk of
recreational PA was associated with a 14% lower risk of all-
cause mortality (HR: 0.86, 95% CI: 0.75–0.98,
p
trend
<
0.0001). Similar results were seen for both walking and
other recreational PA.
The associations of pre- or postdiagnosis recreational PA
with PCSM did not differ by age at diagnosis (
<
70 and 70
yr), BMI (
<
25, 25–
<
30, and 30 kg/m
2
), smoking status
(never and ever), diagnosis year (1992–1998, 1999–2005,
and 2006–2011), or follow-up time (
<
10 and 10 yr for
prediagnosis analyses,
<
6 and 6 yr for postdiagnosis
analyses). Change in PA from pre- to postdiagnosis showed
no clear patterns of associations with PCSM (data not
shown).
4.
Discussion
In this large prospective cohort study of men diagnosed
with nonmetastatic prostate cancer, higher prediagnosis
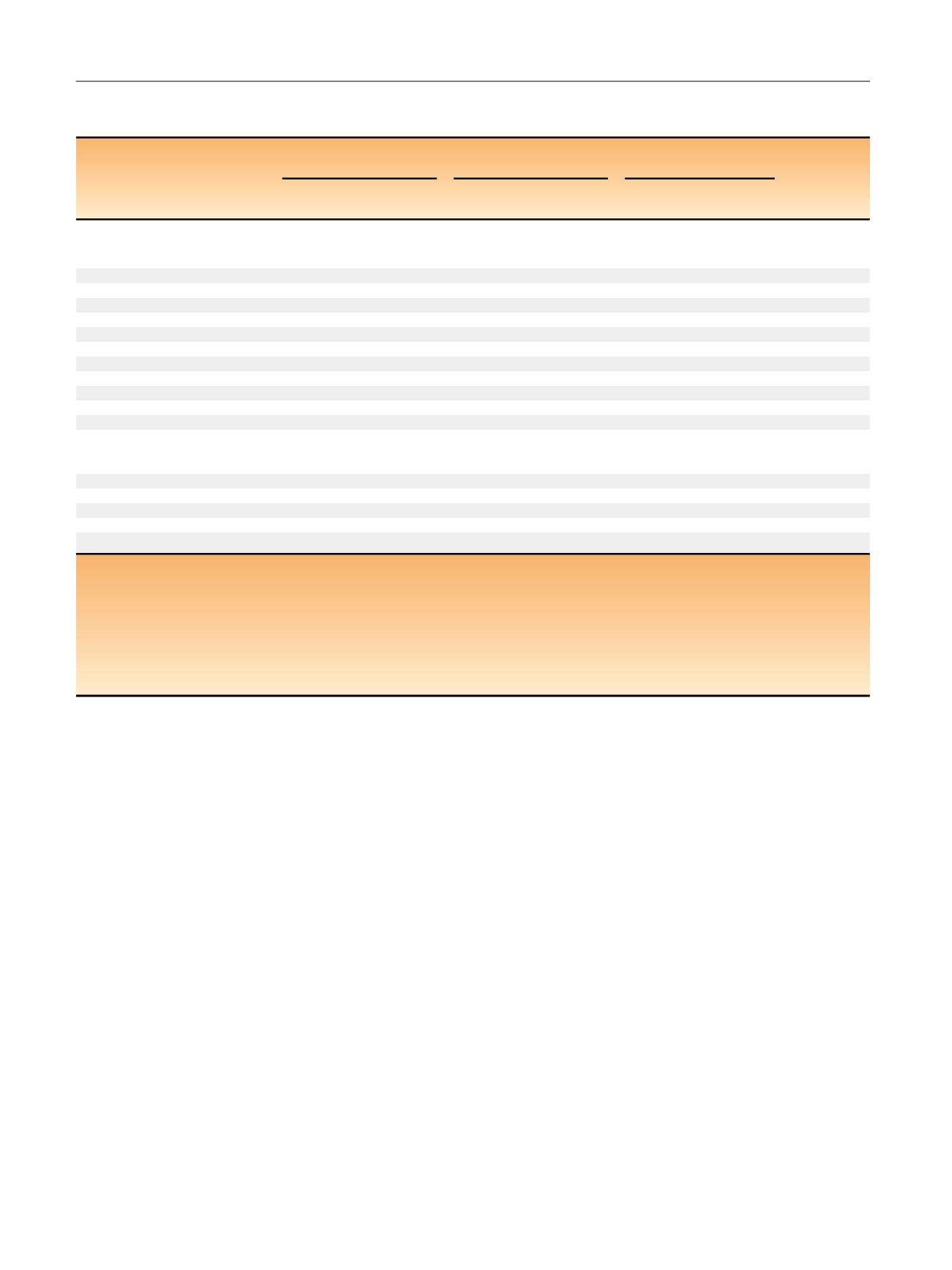
Table 4 – Prostate cancer–specific mortality by postdiagnosis recreational physical activity among men diagnosed with nonmetastatic
prostate cancer in the CPS-II Nutrition Cohort (1992–2012)
Median
MET-h/wk
All prostate
cancer
a[12_TD$DIFF]
Lower-risk prostate
cancer
bHigh-risk prostate
cancer
cp
interaction
Deaths/
person-yr
HR
(95% CI)
Deaths/
person-yr
HR
(95% CI)
Deaths/
person-yr
HR
(95% CI)
Total recreational
physical activity
d[9_TD$DIFF]
(MET-h/wk)
[13_TD$DIFF]
0.1
<
3.5
0.9
45/3079
1.13 (0.77–1.66) 24/2116
1.16 (0.69–1.95) 15/489
1.25 (0.60–2.62)
3.5–
<
8.75
6.8
76/7526
1.00 (ref.)
49/5407
1.00 (ref.)
21/1204 1.00 (ref.)
8.75–
<
17.5
14
63/7462
0.81 (0.58–1.15) 29/5272
0.72 (0.44–1.15) 24/1305 0.77 (0.40–1.49)
17.5+
29.5
77/12 427 0.69 (0.49–0.95) 41/8966
0.67 (0.43–1.04) 28/2084 0.69 (0.37–1.29)
p
trend
0.006
0.04
0.1
Walking
d , e (h/wk)
0.36
<
1
0
60/4915
1.07 (0.77–1.49) 29/3346
0.92 (0.58–1.46) 23/775
1.77 (0.95–3.29)
1–3
7
106/11 679 1.00 (ref.)
68/8504
1.00 (ref.)
28/1832 1.00 (ref.)
4–6
14
52/6866
0.85 (0.60–1.20) 23/4834
0.68 (0.41–1.10) 21/1306 1.10 (0.58–2.06)
7
24.5
43/7034
0.76 (0.53–1.10) 23/5078
0.70 (0.43–1.15) 16/1169 1.01 (0.52–1.98)
p
trend
0.07
0.2
0.2
Other recreational
physical activity
d[14_TD$DIFF]
, f(MET-h/wk)
0.49
<
3.5
0
177/17 758 1.38 (0.96–1.99) 101/12 562 1.62 (0.97–2.69) 57/3 088 1.03 (0.56–1.92)
3.5–
<
8.75
5.5
38/5829
1.00 (ref.)
19/4137
1.00 (ref.)
16/917
1.00 (ref.)
8.75–
<
17.5
12.5
27/3901
1.05 (0.63–1.75) 13/2925
1.06 (0.51–2.20) 11/603
1.01 (0.42–2.41)
17.5+
28
19/3006
1.15 (0.65–2.02) 10/2137
1.23 (0.56–2.70) 4/474
0.51 (0.15–1.71)
p
trend
0.2
0.2
0.3
CPS = Cancer Prevention Study; HR = hazard ratio; CI = confidence interval; MET = metabolic equivalent task; ref. = reference.
a
Includes T1–T2 cancers with unknown Gleason score not included in lower- or high-risk categories.
b
Defined as Gleason score 2–7 and T1–T2.
c
Defined as Gleason score 8–10 or T3–T4 or nodal involvement.
d
Adjusted for age at diagnosis, race, calendar year of diagnosis, tumor extent, nodal involvement, Gleason score, education, family history of prostate cancer,
initial treatment, history of prediagnosis prostate-specific antigen testing, postdiagnosis cardiovascular disease history, postdiagnosis other cancer history,
postdiagnosis body mass index, postdiagnosis smoking status, prediagnosis red meat and processed meat intake, and postdiagnosis sitting time.
e
Further adjusted for other recreational physical activity.
f
MET hours of other physical activity is calculated as total recreational MET hours minus walking MET hours; model further adjusted for walking.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 9 3 1 – 9 3 9
936
















